Condoms: Counseling Tips for Preventing Failure and Reducing Risk
Share
Condoms: Counseling Tips for Preventing Failure and Reducing Risk
When discussing contraception, condoms remain one of the most accessible and widely used options for preventing both pregnancy and sexually transmitted infections (STIs). Still, consistent misuse or misinformation can undermine their effectiveness—even when intentions are good.
This guide offers 5 practical counseling points you can use when working with students, young adults, or anyone seeking accurate, nonjudgmental information about condoms.

1. Reinforce the Importance of Consistent, Correct Use
Condoms are highly effective—when used properly.
- When used correctly every time, condoms are up to 98% effective in preventing pregnancy.
- Misuse is the most common reason for failure, not the product itself.
- Counseling should focus on skill-building rather than fear—how to use, check, and store condoms correctly. Let’s look at a few examples.
2. Normalize Questions About Fit, Feel, and Use
Comfort and correct sizing matter more than people realize.
- Condoms come in different sizes and materials. If they’re too tight, they may break. Too loose? They can slip off.
- Encourage patients to read the packaging and try different brands if needed.
- Discuss latex allergies and the availability of non-latex options.
- If a condom slips or breaks frequently, it’s not just bad luck—adjustments are needed.
3. Address Modern Misconceptions (Especially Online)
“Quick answers” from the internet often miss the context.
- Many patients are unaware that condoms expire and degrade with heat or friction.
- Explain why condoms should never be stored in wallets, cars, or exposed to extreme temperatures.
- Social media trends and online forums often downplay correct usage—correct myths gently and confidently.
- Discourage “double bagging” (wearing two condoms at once), which increases friction and the risk of breakage.
4. Emphasize Long-Term Learning Over One-Time Fixes
Knowing how to prevent failure is better than scrambling after it happens.
- Encourage building knowledge of reliable lubrication (water-based vs oil-based), proper storage, and consistent use before it’s needed.
- Include instruction on how to check for tampering (small punctures, tears) and what to do if the condom slips inside.
- Promote self-advocacy: checking the condom before use, asking for the right size, and not relying on “just the tip” or withdrawal.
- Several medications (such as antibiotics) can make oral contraceptives less effective. You can advise condom use for patients using both of these treatments.
5. Support Emergency Preparedness Without Shame
If something goes wrong, there are options—and acting fast matters.
- Emergency contraception (EC) is most effective when taken as soon as possible—ideally within 72 hours.
- Over-the-counter options like Plan B® are widely available. Ella® is a prescription-only alternative that can be used up to 5 days later.
- Encourage patients to keep EC on hand and normalize having a plan before a mishap occurs.
- Remind them that EC is not an abortion pill and does not affect future fertility, but weight may change how it works in the body..
Final Note for Counselors and Educators
Condom counseling isn’t just about mechanics—it’s about reducing shame, building confidence, and helping patients feel capable of managing their sexual health. As policies shift and misinformation spreads, clear, honest guidance matters more than ever.
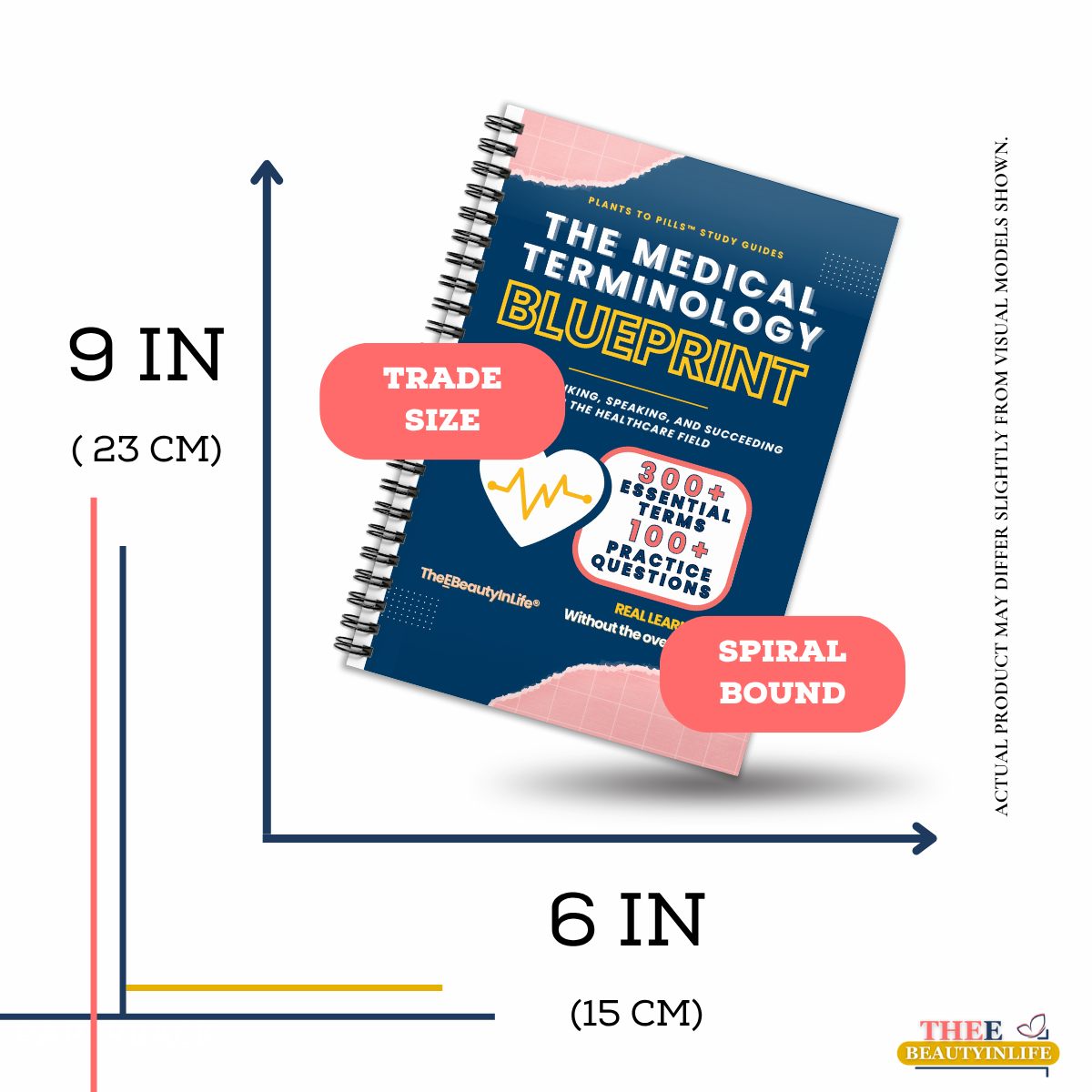
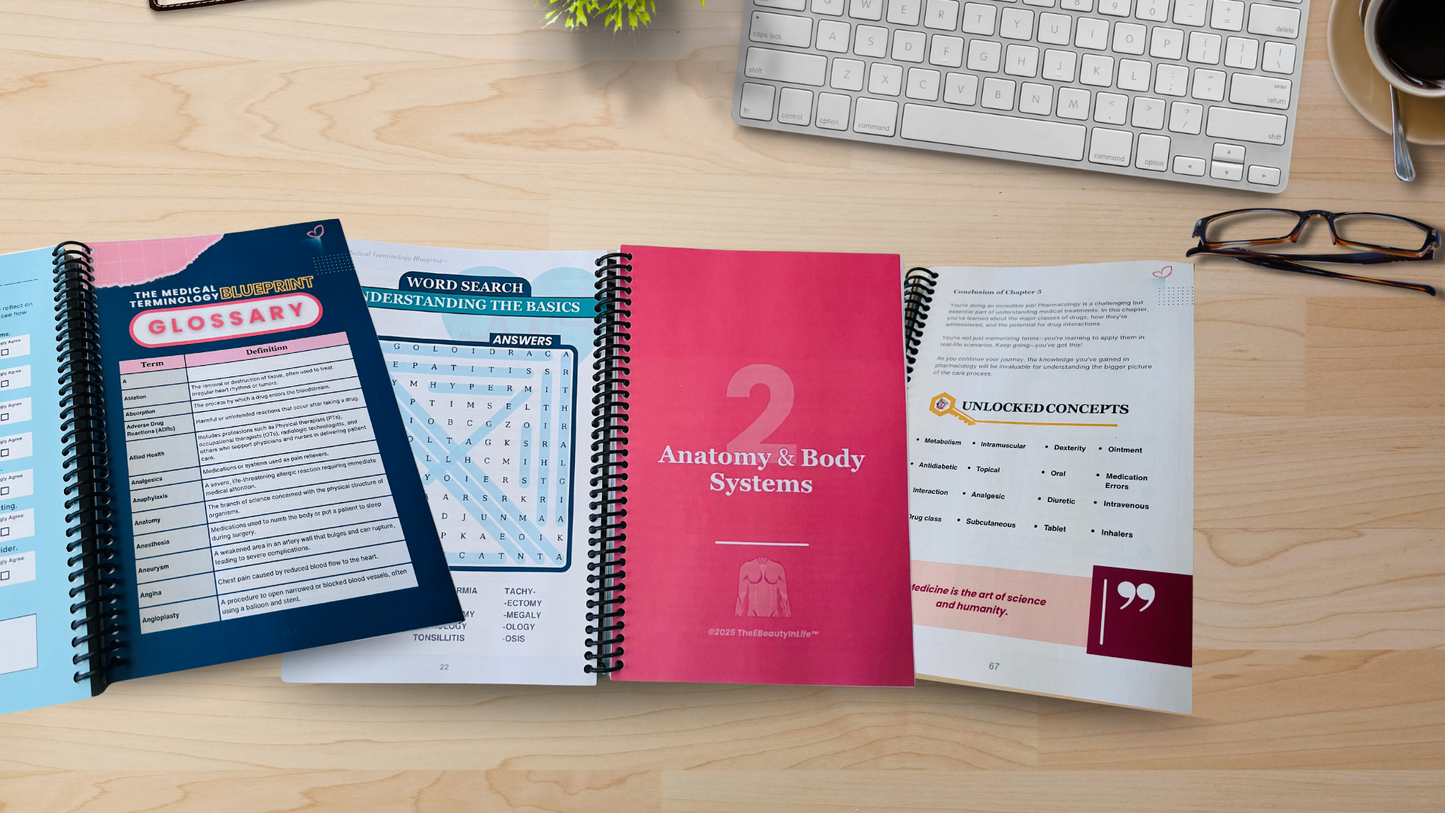
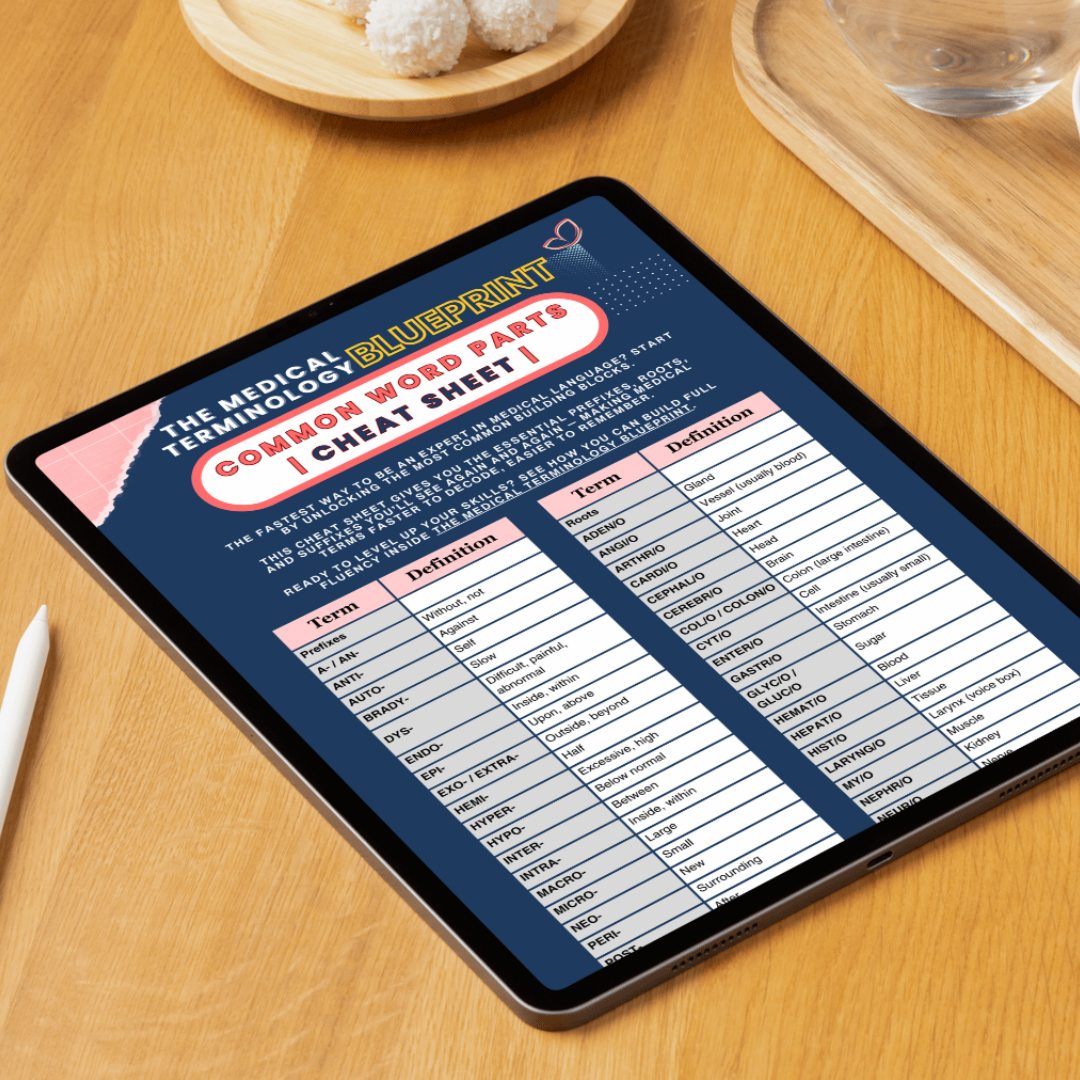
For students looking for clear, judgment-free tools to understanding healthcare concepts like this one: Explore The Medical Terminology Blueprint—built to empower learners with real-world relevance.
Want more tips like this?
Stick around—new posts are upcoming. You can also join the list to get helpful strategies (and a free cheat sheet) delivered straight to your inbox.